#######################
VEDANTASARA
EKB
SUPERIMPOSITION - ENQUIRY
SNAKE V ROPE
WORLD V BRAHMAN
CONSCIOUSNESS TOP DOWN NOT BOTTOM UP
APAVADA
DE-IMPOSITION
############################
IGNORANCE - HAS SRT - TRIGUN - SATWA RAJAS TAMAS
################################
ABRAHAMIC SIN V DHARMIC IGNORANCE
###############################
JIVA- SENTIENT BEING
ISHWARA- GOD OF RELIGN
INSTRUMENTALITY OF MAYA
BRAHMAN IS ONE, MAYA IS MANY
TRUTH IS ONE, LIES ARE MANY
######################################
BIJATIYA VEDA - DIFF OF SPECIES
SAJATIYA VEDA- DIFF BETN HUMANS
SWAGATA VEDA- DIFF IN SAME ENTITY - EYES STOMACH LEGS
###################################
ADVAITA VEDA - ONE BRAHMAN , NO BSS VEDAS
####################################
MONOTHEISM IS HALFWAY- BIJATIYA VEDA STILL THER - GOD V CREATION
####################################
FOREST , RESERVOIR , ONE PRIMAL IGNORANCE
TINY BIT OF IGNORANCE KNOCKS US INTO SAMSARA
###################################
LIMITATION SCHOOL V REFLECTION SCHOOL
AFTER SANKARA
###################################
ISHWARA - CONSCIUSNESS BECOMES GOD
4 NAMES
ABYAKTAM- UNMANIFEST
ANTARYAMI - INNER CONTROLLER
JAGAT KARANAM- CAUSE OF UNIVERSE
ISHWARA- LORD
ROPE + IGNORANCE= SNAKE, GARLAND, CRACK ON EARTH
#################################
CONSC ILLUMINES THE IGNORANCE OF ALL ORGANISMS
TAKEN FROM MANDUKYA UPANISHAD
######################################
MAYA IS LIKE THE UNIFORM OF THE ACTOR
CONSC REQUIRES UNIFORM OF MAYA
NIRGUNA BRAHMAN > SAGUNA BRAHMAN, POWERS GIVEN TO BRAHMAN BY MAYA
######################################
MAYA
AGGREGATE OF IGNORANCE
MAYADHISHA V MAYADHINA
LORD OF MAYA GOD V SUBJECT OF MAYA US
####################################################
BLISS SHEATH OR ANANDAMOY KOSHA
#############################
COSMIC DISSOLN INTO COSMIC SUSHUPTI
SUBTLE MINDS DISSOLVE THER
############################
BRAHMAN- EKB
MAYA- SRT
SATWA- CALM
RAJAS- DYNAMISM
TAMAS- DULLNESS
###########################
SRT IS DYNAMIC
##############################
PRAKRITI
APPEARNCE IS MADE OF SRT- THEY ARE NOT REAL - ADVAITA
############################
U R NOT AN ERROR
U R BRAHMAN
IN ERROR I MA THINKING MYSELF AS A LIMITED SENTIENT BEING
ALL JIVA NARAYAN
BRAHMA SATYAM, JAGAT MITHYA
########################
H- TO FIND OWN BRAHMAN NATURE
#######################
ASHRAYA
SAPTA VIDHAN PRABRITTI
WHERE IS THE IGNORANCE- IN BRAHMAN OR IN JIVA
VARTIKA SCHOOL- IT DOES NOT MATTER
AS BRAHMAN IS AS JIVA
IGNORANCE IS BEGINNIGLESS BUT HAS AN END
EG I DONT KNOW GERMAN , I PICK UP A TEXT BOOK OF GERMAN, IGNORANCE COMES TO AN END
#########################
#########################
B- TO FIND OWN BUDDHA NATURE
########################
MAYA ATITA = NIRGUNA BRAHMAN
#######################
ENLIGHTENED PERSON BEYOND TRIGUNAS - KNOWS HE IS BRAHMAN
#####################
FALSIFIABILITY , MEASURABILITY ARE PARTS OF MAYA
SC INVESTIGATES RELNSHIP BET MAYA OBJECTS
#########################
BRADLEY- ONLY TYPE OF EXISTENCE IS CONSCIOUSNESS
APPEARING TO
########################
VEDANTA IS NOT SOLIPSISM
PRIMACY OF 1ST PERSON PERSPECTIVE
HARD PROBLEM OF CONSCIOUSNESS
#############################
P KZN HTHD
A Teenager With Fever Who Can’t Talk After Visiting Mexico
Editor's Note: The Case Challenge series includes difficult-to-diagnose conditions, some of which are not frequently encountered by most clinicians but are nonetheless important to accurately recognize. Test your diagnostic and treatment skills using the following patient scenario and corresponding questions. If you have a case that you would like to suggest for a future Case Challenge, please contact us.
Background
A 13-year-old girl presents to the emergency department (ED) with 2 months of worsening shortness of breath, malaise, fever, and loose stools. She traveled to Mexico approximately 10 weeks ago; after her trip, she had nonbloody, frequent, loose stools for 2 weeks. She then began having general malaise, with intermittent fevers every 2-3 weeks and dyspnea upon exertion. She reported sporadic shakiness, dizziness, diaphoresis, and tachycardia at rest. She also developed intermittent "burning" head pain and recurrence of loose stools.
She was evaluated by her primary care physician for dyspnea and was prescribed an albuterol inhaler, which had no effect. She had unremarkable pulmonary function testing and chest radiography findings. Inhaled ipratropium, intranasal fluticasone, and omeprazole had no effect. Allergy and otolaryngology specialists believed that her shortness of breath was secondary to vocal cord dysfunction.
Two weeks before her ED presentation, the patient experienced daily fevers for 1 week, with continued loose stools. Her pediatrician obtained stool studies for Salmonella, Shigella, Campylobacter, and Clostridium difficile, which were all negative. No growth on blood and urine cultures was noted, Epstein-Barr serology was negative, and a tuberculin skin test was nonreactive.
The patient was started on amoxicillin for 10 days for presumed sinusitis. Her fever ceased on day 2 of antibiotics but returned, with a temperature as high as 103°F (39.4°C) on day 8 of antibiotics, 3 days before her ED presentation. She continued to have up to four loose stools per day. Her headache became more severe and began to awaken her from sleep. She denied upper respiratory infection (URI) symptoms, cough, rash, night sweats, or persistent weight loss. She presented to the ED owing to worsening symptoms and persistent fevers.
Her family history is significant for a paternal grandmother with a rheumatologic disorder and a father with a resected thyroid mass; the etiology of both is unknown. Her social history is unremarkable, other than her recent travel to Mexico and exposure to a dog at home.
Physical Examination and Workup
Upon physical examination, the patient's temperature is 98.2°F (36.8°C), blood pressure is 133/81 mm Hg, heart rate is 145 beats/min, respiratory rate is 36 breaths/min, oxygen saturation is 100% in room air, and weight is 71.65 lb (32nd percentile). She appears nontoxic. Her head and neck examination is unremarkable, other than tenderness of the bilateral temporal areas. She is tachycardic, with normal S1 and S2 sounds and no murmurs. She is tachypneic, with clear lungs throughout and no accessory muscle use. Mild generalized abdominal and chest tenderness are present, with a soft abdomen and no guarding or rebound.
Preliminary laboratory findings are notable for a white blood cell count of 16,200/µL, hemoglobin level of 10.9 g/dL, platelet count of 309,000/µL, erythrocyte sedimentation rate of 23 mm/h, and C-reactive protein level of 3.7 mg/dL. Her electrolyte and liver enzyme findings are unremarkable. Blood culture results are pending, and urinalysis is negative. She is admitted for further evaluation of her fever of unknown origin.
The next morning, the patient develops a fever (100.8°F [38.2°C]), with persistent resting tachycardia (142 beats/min) and tachypnea, even while afebrile. She has abdominal pain, loose stool, and an episode of vomiting. She continues to have headache, which awakens her from sleep. Upon examination, she has new-onset disorientation, with word-finding difficulty.
A brain MRI is obtained; it was substantially limited by artifact from the patient's braces but otherwise revealed no acute intracranial abnormality (Figure 1).
Figure 1.
Lumbar puncture is performed, and initial cerebrospinal fluid studies are negative, including cell count, differential, and Gram stain. Pediatric rheumatology and infectious disease specialists are consulted.
Discussion
The patient's screening thyroid studies revealed a thyroid-stimulating hormone (TSH) level < 0.01 mIU/L, free triiodothyronine (T3) level > 20 pg/mL, and total thyroxine (T4) level > 29 µg/dL. Upon repeat examination, she was found to have a mildly enlarged diffuse goiter, which was previously unrecognized.
Hyperthyroidism in children and adolescents is relatively rare, occurring in 0.1-3 per 100,000 children; 95% of these patients are diagnosed with Graves disease.[1,2] As seen in the patient in this case, Graves disease is more common among females, with a peak incidence at age 10-15 years.[1] Graves disease involves the infiltration of lymphocytes into the thyroid gland and production of stimulating autoantibodies to the TSH (thyrotropin) receptor. These thyroid-stimulating immunoglobulins (TSIs) mimic the action of TSH, causing uninhibited production and release of thyroid hormones. This results in increased T3 and T4 levels and suppression of TSH.[1-3]
Patients typically present with weight loss, frequent stools, fatigue, palpitations, dyspnea, anxiety, emotional lability, and warm, moist skin.[3] Signs and symptoms of hyperthyroidism are similar in children and adolescents to those in adults. However, a considerable delay in diagnosis often occurs in children, ranging from 5 months in pubertal children to 8 months in prepubertal children.[2] Often, behavioral disorders, including attention-deficit/hyperactivity disorder or anxiety, respiratory diseases (eg, exercise-induced asthma), or primary cardiac diseases, are considered rather than hyperthyroidism as the cause of the symptoms.
Graves disease is definitively diagnosed by elevated T3 and T4 levels; suppressed TSH levels (< 0.1 mIU/L); elevated thyroid-stimulating antibody titers; and an ultrasound that reveals heterogeneous, hypoechoic tissue with increased blood flow.[1] Thyroid peroxidase antibodies may also be positive in as many as 10% of patients with Graves disease.[3] Radioactive iodine uptake scans show diffuse increased uptake throughout the thyroid gland (Figure 2).
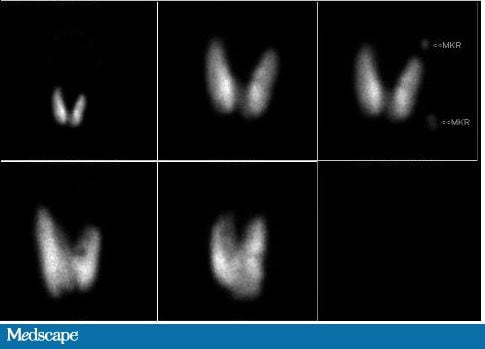
Figure 2.
Many uncommon causes of hyperthyroidism in adolescents are noted. Disorders with a similarly depressed TSH level include activating mutations of the TSH receptor and McCune-Albright syndrome, which is characterized by endocrine system hyperfunction, café au lait macules, precocious puberty, and fibrous dysplasia. Toxic adenomas, toxic multinodular goiter, drug-induced thyroiditis, subacute thyroiditis, and the thyrotoxic phase of Hashimoto thyroiditis can also have suppressed TSH levels and hyperthyroidism. However, these are all distinguished from Graves disease by lack of elevated TSIs and differences in radionucleotide uptake scans. Conditions with release of preformed thyroid hormone, such as subacute thyroiditis, demonstrate decreased radioactive iodine uptake.[3]
Thyroid storm is rare, occurring in less than 1% of adults with hyperthyroidism and an unknown number of children.[2] It is characterized by multisystem organ failure with gastrointestinal manifestations (nausea, vomiting, diarrhea, hepatic dysfunction), cardiovascular manifestations (tachycardia, arrhythmias, hypotension, congestive heart failure), and central nervous system manifestations (agitation, delirium, psychosis, stupor, coma), as well as hyperpyrexia. Thyroid storm is typically seen in patients with known thyroid disease after acute illness, surgery, abrupt cessation of antithyroid medications, or rarely after radioactive iodine therapy.[3] However, thyroid storm can occur from prolonged untreated hyperthyroidism, and the general practitioner needs to remain aware of common symptoms of thyroid dysregulation as well as thyrotoxicosis or thyroid storm.
Treatment for hyperthyroidism in pediatric patients involves antithyroid drug therapy with methimazole (the only approved treatment in the United States for children and adolescents) or propylthiouracil or carbimazole.[1,2] These medications inhibit synthesis of thyroid hormone but may take several weeks to normalize thyroid hormone values. Patients with significant symptoms or thyrotoxicosis are started on beta-blockers to minimize adrenergic effects, such as tachycardia and hypertension.[3] Definitive therapy, with a goal to become hypothyroid, involves either radioiodine ablation or total thyroidectomy.
Graves ophthalmopathy is a significant complication and involves inflammatory infiltrates and edema in retro-orbital tissue, which results in classic proptosis and diminished ocular muscle function. Symptoms of Graves ophthalmopathy are much more mild in children than in adults, and decreased vision is rare.[3] Other complications of Graves disease include thyroid storm, which can be fatal, and medication or surgical side effects.
The patient was initially hospitalized for an unclear etiology of her symptoms and fever of unknown origin. Although many fevers of unknown origin are ultimately infectious in nature, accounting for more than 60% of pediatric cases, recognizing other potential causes is important.[4] These include oncologic, autoimmune, endocrine, inflammatory, or neurologic conditions, which are important to recall in developing a differential diagnosis for fever of unknown origin.
This case represents a diagnosis that was initially delayed because of practitioners' bias toward fever representing an infectious cause, especially with the red herring of preceding international travel. Heuristic biases are "rules of thumb" and shortcuts used in clinical decision-making.[5] Heuristics are often appropriate; these mental shortcuts are developed by pattern recognition and allow practitioners to quickly associate symptoms with a common diagnosis. However, heuristic biases may lead to an incorrect or delayed diagnosis, as in this case. Using heuristics here, infection was considered to be most likely in a patient presenting with fever and diarrhea with recent international travel. However, this patient presented with thyrotoxicosis bordering on thyroid storm.
The pediatric endocrinology service was immediately consulted, and the patient was started on beta-blocker therapy with propranolol. Her tachycardia, fevers, and head pain all improved. Neck ultrasonography revealed a diffusely enlarged thyroid with no nodules. Nuclear medicine thyroid imaging showed toxic diffuse goiter consistent with Graves disease. TSI levels later returned elevated. Propranolol was uptitrated during her hospital stay, and she was started on methimazole. The patient was discharged home on hospital day 4, with great improvement in her symptoms.
The patient has been followed by an endocrinology specialist for her Graves disease and currently remains on medical therapy with low-dose methimazole. She is also being followed by an ophthalmology specialist for mild Graves eye disease. She has been euthyroid with resolution of presenting symptoms, including poorly recognized symptoms such as anxiety and even flawed hand-writing. She may require surgery in the future, because she is not a candidate for radioactive iodine therapy given her eye disease, but she is currently doing well over 1 year after diagnosis.
Question 1 of 2
Frequent loose stools are associated with hyperthyroidism; other symptoms include weight loss, failure to thrive, heat intolerance, attention-deficit/hyperactivity disorder or anxiety, and dyspnea with fatigue. Diagnosis of hyperthyroidism is often considerably delayed in children, even though the symptoms are similar to those in adults.
Question 2 of 2
Beta-blockers (eg, propranolol) should be immediately started to reduce adrenergic effects. At higher doses, propranolol may also reduce peripheral conversion of T4 to T3.[6] Methimazole is used as an antithyroid drug, but it has a delayed onset of action and is not necessarily used for immediate symptom control. Propylthiouracil is also an antithyroid drug but is not recommended as a first-line agent for use in children owing to hepatotoxicity.
References
Hanley P, Lord K, Bauer AJ. Thyroid disorders in children and adolescents: a review. JAMA Pediatr. 2016;170:1008-1019. Source
##############################
BARTONE
Aesthetic pleasure is good pleasure. It’s pleasure that has some deeper meaning than just addictive gratification. Aesthetic pleasure challenges as much as it satisfies. I need more challenging, visceral art, a more challenging and deeply felt aesthetic experience. Something in the symbolic realm that points to an experience of the REAL.
What is the REAL? It’s simply being here, being alive, that’s the real. Being born is real, living is real, dying is real. What if dukkha wasn’t craving or suffering, but the existential REAL of being alive, the sharpness of it? The angst, the agita of simply living another day? What if that is what we have to contend with, not by numbing out, but by simply and totally accepting it as a condition of being alive?
Losing weight could help stave off brain aging, DWM
#################
Most individuals infected with mild-to-moderate COVID-19 have the ability to neutralize the SARS-CoV-2 virus that is responsible.
Contrary to the media panic suggesting that antibodies against the coronavirus fade swiftly, a new Mount Sinai study proves otherwise.
In fact, more than 90 percent of recovered patients produce a strong antibody response lasting for a long time after infection.
DWM
####################
"The whole language of writing for me is finding out what you don’t want to know, what you don’t want to find out. But something forces you anyway."
-- James Baldwin, The Paris Review
#########################
PEACE V STRESS
The biggest difference between peace and stress is attitude. It’s all about how you look at a situation and what you decide to do with it. It’s remembering that there are no certainties in life; we don’t know exactly what the future will bring. So your best strategy for living is to make the best and most positive use of the present moment, even when it disappoints you....
############################
Through others, we become ourselves. -Lev Vygotsky, psychologist (17 Nov 1896-1934)
#############################
ANIMALS DENIED A MEANINGFUL LIFE BY HUMANS
##############################

No comments:
Post a Comment